Anorexia nervosa is a perilous eating disorder marked by an intense fear of gaining weight, an aversion to food, and profound disturbances in self-image. It is far more than a mere diet gone awry; it’s a condition that deeply affects psychological well-being and often coexists with severe anxiety and depression. The consequences can be devastating, including malnutrition and a heightened risk of mortality. Contemporary research is beginning to shed light on the neurobiological underpinnings of this complex disorder, hinting that changes in neurotransmitter activity in the brain may play a pivotal role in its development.
Recent studies suggest that alterations in neurotransmitter systems, particularly those involving the mu-opioid receptors (MOR), may contribute to the development and persistence of anorexia nervosa. These receptors form part of the brain’s intricate opioid system, which is heavily involved in regulating both appetite and pleasure associated with food consumption. Researchers found that individuals with anorexia exhibited increased MOR availability in the brain’s reward processing centers. This observation indicates that their brains are potentially wired differently compared to healthy individuals, creating a heightened sensitivity to food and weight concerns that influences their restrictive eating behaviors.
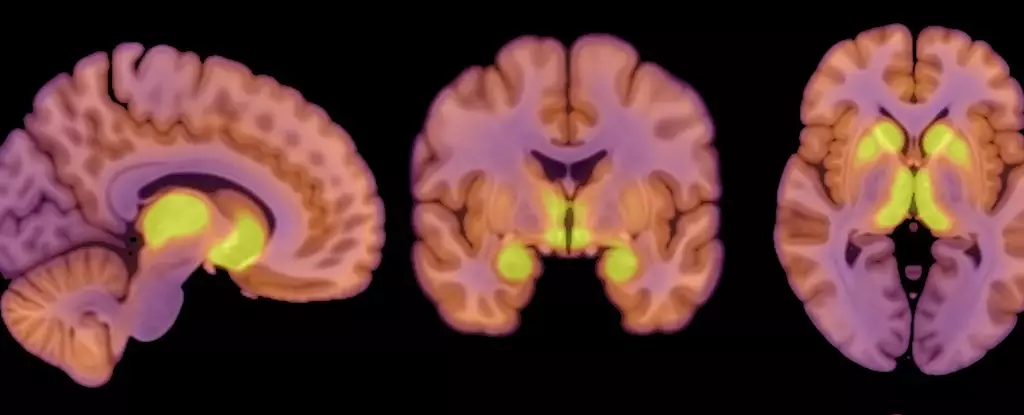
The recent study involved 13 female patients with anorexia, aged between 18 and 32 years, all of whom had a body mass index (BMI) below 17.5. The researchers compared these subjects to a control group of 13 women with BMIs ranging from 20 to 25 and no history of eating disorders. Using positron emission tomography (PET) scans, the research team measured the availability of MORs and analyzed glucose uptake in these patients. Interestingly, despite the significant restriction of caloric intake in anorexia patients, their brains displayed a similar glucose utilization rate to that of the healthy controls. This suggests a protective mechanism that prioritizes brain functionality despite the precarious state of their physical health.
Findings from the study lead to crucial implications about energy distribution within the body, particularly under conditions of malnutrition. It appears that the brain, an organ that typically consumes a considerable portion of a person’s total energy (about 20%), persists in demanding its requisite energy for optimal functionality. Researchers highlighted that the brain establishes a sort of “hierarchy” in energy conservation, ensuring it receives adequate glucose even when the supply is limited due to anorexia. Such a protective mechanism raises questions about how the brain can sustain its functions in the face of severe undernourishment.
The elevated MOR availability in anorexia presents a paradox when contrasted with obesity—a condition characterized by lowered opioid receptor activity. This dichotomy suggests that the body’s endogenous opioid system could be a critical factor in understanding the dynamics of appetite regulation in both extremes of the eating spectrum. Previous research indicates that weight loss can boost MOR levels, adding another layer of complexity to the understanding of this disorder’s neurobiological aspects.
While the study enriches our understanding of anorexia nervosa, it does come with limitations. For instance, the inclusion of only females poses questions about the applicability of the results to male populations, which also experience this disorder, albeit less frequently. Additionally, the small sample size may limit the generalizability of the findings. The absence of a questionnaire assessing eating behaviors further complicates the connection between MOR availability, glucose metabolism, and actual eating habits in patients struggling with anorexia. Future research must strive to explore these relationships more thoroughly and investigate whether changes in the opioid system are the catalyst or a consequence of this eating disorder.
As scholarship continues to articulate the biochemical pathways involved in anorexia nervosa, it is essential to approach treatment and understanding from a more holistic perspective. This disorder does not merely manifest as a diet or lifestyle choice; it represents a complicated interplay of psychological, neurological, and societal factors. Continued investigation into the facets of the brain’s reward systems, including the mu-opioid receptors, holds promise for developing more effective therapeutic interventions and enhancing overall knowledge of this challenging condition. In recognizing that the brain’s regulation of appetite and mood can shape both obesity and the low weight characteristic of anorexia, researchers may find new pathways to support those affected by this debilitating disorder.