For decades, the scientific consensus positioned glycogen primarily as the body’s energy reserve, relegated to roles within the liver and muscles. Its presence in the brain was largely overlooked or dismissed as a mere backup fuel. However, emerging research radically challenges this notion, suggesting that glycogen plays a far more vital and active part in neuronal health and disease than previously appreciated. This revelation underscores how much we still underestimate the intricacies of metabolic processes within the brain and opens a promising frontier for therapeutic development against neurodegenerative diseases like Alzheimer’s.
The recent findings derived from studies at the Buck Institute for Research on Aging exemplify how shifting perspectives on biological functions can ignite breakthroughs. Instead of simply serving as an energy store, glycogen appears to be intricately involved in the pathology of neurons, especially under stressful conditions such as tauopathies—a class of neurodegenerative disorders characterized by abnormal tau protein accumulation. This newfound understanding calls into question long-held assumptions and compels scientists to rethink how brain metabolism influences disease progression.
The Hidden Intersection of Glycogen and Tau Pathology
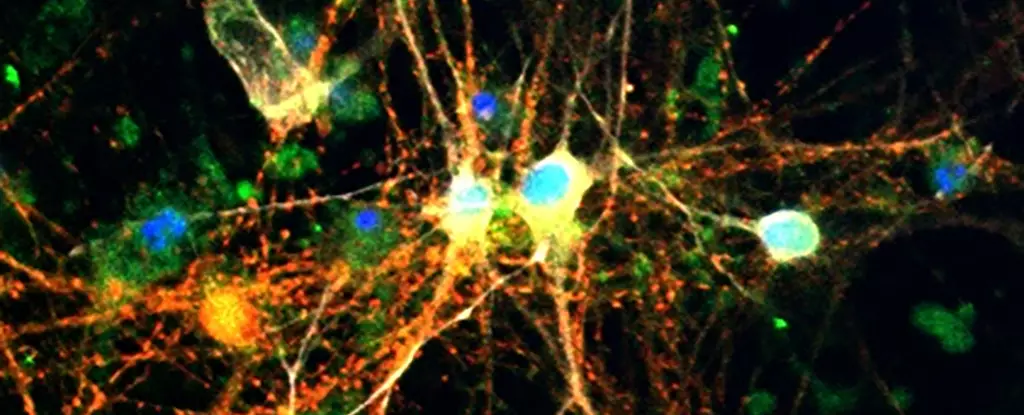
The research reveals a troubling link between excess glycogen accumulation and tau-related neurodegeneration. Using model organisms like fruit flies, or *Drosophila melanogaster*, alongside human brain tissue, scientists observed elevated glycogen levels coinciding with tau build-up. Even more compelling was the discovery that tau proteins interfere with normal glycogen metabolism, disrupting the enzymatic processes that allow glycogen to be safely broken down for use. This disruption results in a dangerous cycle: glycogen accumulates abnormally, exacerbating neuronal stress and damage, thereby accelerating disease progression.
What makes this interaction so critical is the role of glycogen phosphorylase (GlyP)—the enzyme responsible for mobilizing glycogen’s stored energy. When researchers enhanced GlyP activity in tauopathy models, they observed a reduction in glycogen buildup, leading to improved neuronal resilience. The health benefits extended beyond mere biochemical correction; neurons became better equipped to neutralize reactive oxygen species—harmful molecules that contribute to oxidative stress and cell death—ultimately prolonging the lifespan of the model organisms.
This mechanistic insight offers a paradigm shift: if glycogen accumulation worsens neurodegeneration, then manipulating its metabolism could serve as a powerful therapeutic tool. The idea that enhancing the brain’s ability to manage its glycogen stores can reduce pathology places metabolic regulation at the forefront of neurodegenerative treatment strategies, rather than solely focusing on protein aggregation or inflammation.
Diet, Enzymatic Activation, and Future Pharmacotherapy
From these compelling biological insights, the research team explored non-invasive methods to modulate glycogen metabolism, discovering that dietary interventions might make a tangible difference. Specifically, imposing a low-protein diet—already known for its benefits in overall health and longevity—appeared to activate metabolic pathways that increased GlyP activity. This dietary restriction translated into longer survival times and less neural damage in tauopathy models, suggesting that calorie or nutrient management could be part of a holistic approach to delaying neurodegeneration.
Even more exciting is the development of pharmacological agents that replicate these beneficial effects. The scientists crafted drugs based around molecules like 8-Br-cAMP, which act as cellular signaling mimetics, promoting glycogen breakdown. These drugs demonstrated efficacy similar to dietary restriction, hinting at a future where tailored therapies could manipulate brain glycogen dynamics pharmacologically. Targeting specific enzymes like GlyP sidesteps the need for strict diets, offering a more precise and potentially more effective intervention.
The implications extend further when considering existing medications such as GLP-1 receptor agonists exemplified by Ozempic. Originally designed to manage diabetes and promote weight loss, these drugs may already exert secondary protective effects on the brain by influencing glycogen pathways. This intersection suggests a promising repurposing of current drugs as neuroprotective agents, broadening the scope of metabolic therapies against Alzheimer’s and related disorders.
A New Perspective on Neurodegeneration and Aging
Ultimately, recognizing glycogen’s active role in neuronal health symbolizes a profound shift in how we view brain aging and disease. The findings argue that metabolic imbalances—specifically relating to glycogen management—are not mere consequences but potential drivers of pathology. By targeting these fundamental processes, scientists are inching closer to innovative treatments that address root causes rather than just symptoms.
The integration of metabolic regulation into neurodegeneration therapy challenges the traditional focus on amyloid plaques and tau tangles alone, urging a broader, more holistic view. It prompts questions about how lifestyle choices, diet, and existing medications could be harnessed or optimized to maintain neuronal glycogen balance, potentially delaying or even preventing the onset of debilitating conditions like Alzheimer’s. As research deepens, the possibility of transforming metabolic pathways into therapeutic targets heralds a new era where brain health is safeguarded from the inside out—through the mastery of sugars stored deep within neurons.