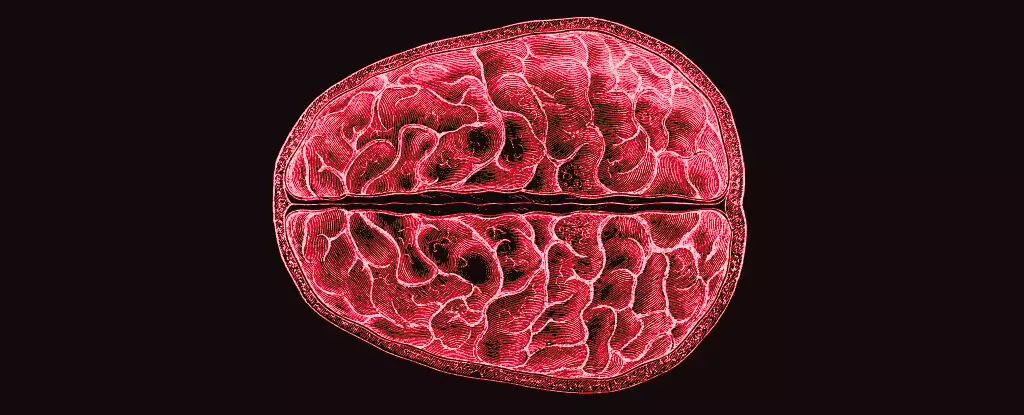
Hormones are often painted as mere regulators of bodily functions, yet their influence runs far deeper, extending to complex realms such as cognitive function, emotional stability, and even our very understanding of ourselves. Recent research pioneered by neuroscientists Elizabeth Rizor and Viktoriya Babenko at the University of California Santa Barbara advances our grasp of this connection, uncovering profound insights into how hormonal fluctuations during the menstrual cycle can reshape not only behavior but also the structural integrity of the brain itself.
The significance of these findings cannot be overstated. For those who menstruate, experiencing around 450 cycles over a lifetime constitutes a substantial portion of their existence, yet, unexpectedly, scientific inquiry into the neuropsychological ramifications of menstruation has been relatively scant. Why is there a lack of research when the effects of these natural cycles govern so much of daily life? The answer remains elusive, but this oversight speaks volumes to the broader societal tendency to ignore women’s health issues—an ignorance that this study bravely begins to challenge.
Research Breakthroughs: Beyond Traditional Boundaries
Utilizing advanced MRI scanning techniques, the study encompassed three distinct menstrual phases: menstruation, ovulation, and the mid-luteal phase. By closely tracking the hormonal profiles of thirty participants alongside their brain structures, Rizor’s team uncovered simultaneous changes across brain regions not typically associated with hormonal fluctuations. Their findings contradict prevailing notions that alterations in brain structure are confined to well-understood systems, specifically those involving the hypothalamic-pituitary-gonadal (HPG) axis. The suggestion that widespread brain changes occur suggests a holistic integration of hormonal effects, which invites further inquiry into how these fluctuations influence cognitive function and emotional well-being.
Interestingly, the research illustrates that changes in white matter microstructure—those essential highways for neuronal communication—occur alongside fluctuations in hormone levels. For instance, the surge of estrogen just prior to ovulation correlates with observable advancements in white matter health, indicating faster neurological processing at a time of heightened fertility. This observation raises compelling questions about cognitive enhancement in relation to hormonal cycles and whether specific life decisions or emotional responses could be contextually influenced by the dynamics of one’s menstrual cycle.
The Underestimated Influence of the Menstrual Cycle
It’s essential to recognize that the societal dialogue surrounding menstruation has often relegated the topic to stigma and silence. The fact that hormonal fluctuations during the menstrual cycle can lead to substantial brain and mood changes opens up discussions about the necessity for workplace policies, educational frameworks, and healthcare models to account for such variations. As Rizor and Babenko pointed out, conventional research has often fixated on observable behavior rather than delving into the underlying structural changes, leaving a considerable gap in our understanding.
The implications of these findings are particularly noteworthy when considering the mental health challenges faced by many who menstruate. Conditions like premenstrual dysphoric disorder (PMDD) show how hormonal shifts can lead to profound emotional disturbances. Recognizing that these fluctuations possibly alter brain structures may provide new avenues for treatment and support systems, which remain critically underexplored within mainstream medicine.
Future Directions: Implications for Mental Health
The convergence of hormonal cycles with structural brain dynamics suggests a rich field of exploration for future research. Questions about why certain women may experience extreme psychological effects during their menstrual cycles become pertinent. With data showing shifts in gray and white matter volumes, as well as cerebrospinal fluid, there is potential to forge connections between these physiological changes and behavioral outcomes.
Moreover, as society evolves towards a more comprehensive understanding of mental health, the demand for tailored approaches that acknowledge the cyclical nature of hormonal influences on well-being will only grow. Education about how menstruation impacts brain health is crucial—offering insights that could foster empathy, transformation, and improved environments for those affected. The time has come to lift the veil on the biological realities of menstruation, embracing a nuanced understanding that underpinning physiological trends greatly inform psychological health.
In essence, the revelations from this study advocate for not only greater awareness but also prompt systemic changes across disciplines—from healthcare to social policy. Understanding the mind-body connection through the lens of the menstrual cycle is not simply a matter of scientific curiosity; it speaks to the fundamental respect and acknowledgment that half of the global population deserves.