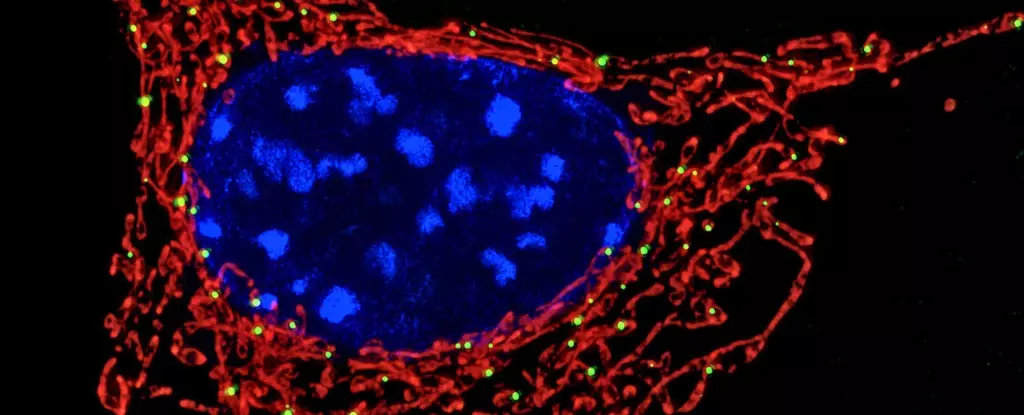
For decades, mitochondria were relegated to a singular role: the cell’s powerhouses, churning out the energy needed to sustain life. Yet emerging research reveals that these tiny organelles extend far beyond mere energy generators. They play a pivotal role in orchestrating complex immune responses. Far from passive energy suppliers, mitochondria have become central players in how our immune system detects, reacts to, and neutralizes microbial threats. This evolving perspective shifts our understanding of cellular biology, linking metabolism directly to immune function in ways previously unappreciated.
Sensing Bacterial Metabolism: A New Frontier in Immunity
One of the most startling discoveries is mitochondria’s capacity to ‘listen in’ on bacterial metabolic byproducts, specifically lactate. Lactate, far from being just a marker of muscle fatigue, serves as a crucial message within the infected cell. Many bacteria excrete lactate as a result of their own metabolic processes. When neutrophils—our immune system’s first responders—engulf bacteria in phagosomes, the mitochondria within these cells detect the accumulation of lactate. This signal isn’t trivial; it acts as a distress call that bacterial killing mechanisms alone may be insufficient, triggering a specialized immune strategy.
Neutrophil Extracellular Traps: The Immune System’s Sticky Snare
The process mitochondria initiate involves the formation of neutrophil extracellular traps (NETs). These intricate webs, composed of DNA and antimicrobial proteins, work like sticky snares to immobilize and neutralize invading microbes. Previously, NET formation was largely attributed to signals related to cell stress or damage. The revelation that mitochondria respond specifically to bacterial lactate to trigger NET release challenges this view and adds a metabolic dimension to immune activation.
What makes this pathway particularly fascinating is the spatial separation within the cell: bacteria reside within phagosomes, isolated compartments, yet mitochondria outside these structures can ‘sense’ their presence. This points to a sophisticated molecular dialogue between compartments at the cellular level, hinting at highly evolved mechanisms ensuring swift and targeted immune responses.
Implications for Autoimmunity: The Lupus Connection
This mitochondrial sensing mechanism sheds light on perplexing immune deficiencies observed in autoimmune diseases, notably systemic lupus erythematosus (SLE). Lupus patients suffer from an overactive immune system yet paradoxically are more prone to infections. This apparent contradiction becomes clearer when considering mitochondrial dysfunction in neutrophils from these patients. Their mitochondria fail to detect bacterial lactate properly, leading to impaired NET formation and a diminished capacity to trap bacteria. The result is a weakened frontline defense despite systemic immune overactivity. This insight reposition mitochondria as crucial arbiters balancing immune vigilance with restraint—a role critical to maintaining immune homeostasis.
Bridging Metabolism and Immunity Through Mitochondria
This field, often referred to as immunometabolism, is redefining biological dogmas by positioning metabolism as not merely supportive but directive in immune function. Mitochondria, at the heart of cellular metabolic pathways, act as sensors and regulators, integrating metabolic cues to modulate immune responses dynamically. Such findings are radical because they argue against a simplistic energy-only function for mitochondria and instead champion their role as immune command centers.
Therapeutic Horizons: Modulating Mitochondrial Sensing
Recognizing mitochondria’s role in immune sensing opens promising therapeutic avenues. For individuals with compromised immunity, such as those with lupus or other chronic conditions, strategies to enhance mitochondrial lactate sensing could strengthen their ability to produce NETs and control infections more effectively. Conversely, conditions that involve excessive NET formation—contributing to tissue damage as seen in severe COVID-19 or autoimmune flares—might benefit from damping these mitochondrial signals to prevent unnecessary harm.
Moreover, this discovery raises provocative questions about whether other immune cells utilize similar metabolic cues and whether additional microbial metabolites function as immune activators. Unlocking these mechanisms could lead to the development of targeted therapies that finely tune immune responses, enhancing defense against pathogens while minimizing collateral tissue damage.
The Immune System’s Metabolic Watchtower
Mitochondria are redefining themselves from simple cellular energizers into vigilant sentinels that monitor the metabolic landscape within our cells. Their ability to detect subtle bacterial signals such as lactate highlights an intricate evolutionary adaptation, equipping immune cells to make rapid, informed decisions in the face of infection. It’s a compelling reminder that cellular metabolism and immunity are intertwined at a level that demands reconsideration of how we approach infectious disease, autoimmunity, and immune modulation in future research and clinical applications. This evolving understanding not only broadens basic biological knowledge but also paves the way for innovative treatments that harness the mitochondria’s full potential in immune defense.