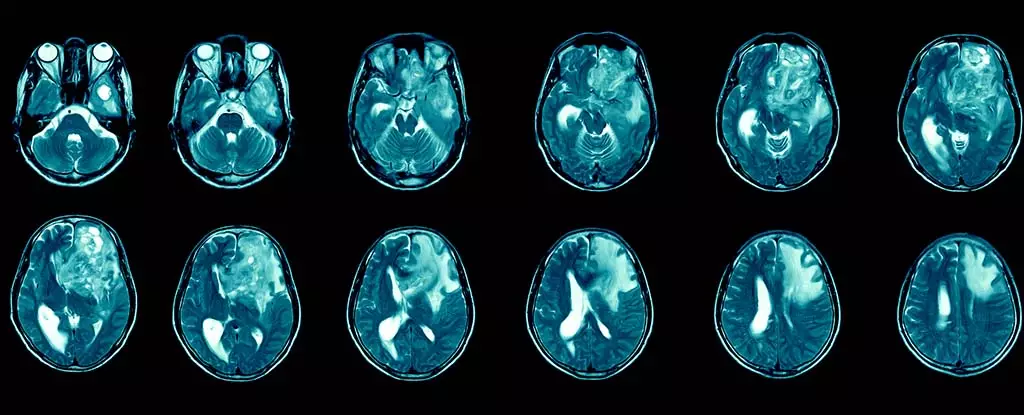
Glioblastoma is a formidable adversary in the realm of brain cancer, representing both the most prevalent and lethal form of this disease. Patients diagnosed with glioblastoma often face disheartening prognoses, with median survival durations hovering merely between 12 and 15 months post-diagnosis. Alarmingly, the survival rate extends beyond five years for less than 7% of patients, underscoring the urgency for innovative treatment approaches. Despite these formidable statistics, the impact of glioblastoma extends beyond mere survival; patients grapple with debilitating symptoms that severely diminish their quality of life, including persistent headaches, seizures, and various cognitive and emotional alterations.
Glioblastoma belongs to a class of tumors referred to as gliomas, which originate in the supportive tissue of the brain and spinal cord. As classified by the World Health Organization, glioblastoma is designated a grade 4 tumor, characterized by its aggressive proliferation and invasive capabilities. In the UK, around 3,200 new glioblastoma cases are identified annually, contributing to a total of 12,700 brain and central nervous system tumors diagnosed each year. On a global scale, the incidence ranges from approximately 3.2 to 4.2 cases per 100,000 individuals each year, amounting to an estimated 150,000 new cases worldwide.
Standard treatment methodologies such as surgical intervention, chemotherapy, and radiation often yield only temporary respite. Glioblastoma’s inherent resilience is attributable to its ability to evade immune responses and the formidable blood-brain barrier, which acts as a physiological blockade to many therapeutic agents. Surgical removal of the tumor frequently leads to recurrence, emphasizing the pressing need for more sustainable treatment solutions.
In recent years, research into immunotherapy has surged, offering a glimmer of hope in addressing glioblastoma’s challenges. This innovative form of treatment leverages the body’s immune system to selectively target and eliminate cancer cells, a paradigm shift in cancer therapy. While immunotherapy has shown promise in treating other cancer types, including melanoma and non-small cell lung cancer, its applicability to glioblastoma remains complex due to the tumor’s unique adaptive characteristics.
What complicates glioblastoma treatment further is the tumor’s heterogeneity, with distinct genetic mutations manifesting in various regions. Nonetheless, optimism persists within the scientific community as recent studies demonstrate the potential of delivering immunotherapy via injections into the cerebrospinal fluid. This method seeks to bypass the blood-brain barrier and more directly engage the tumor.
Despite the excitement surrounding immunotherapy, several hurdles remain in translating its potential into actionable solutions for glioblastoma patients. Historically, funding challenges have stymied brain cancer research. However, concerted efforts are now underway to attract talent from diverse research disciplines to contribute fresh perspectives on glioblastoma treatment.
My personal journey in this field spans over two decades, grounded in exploring immune modulation in chronic infections and cancer. Recently, my focus has shifted to understanding the intricate communication between immune cells and brain function, particularly regarding neurodegenerative diseases like Alzheimer’s. Armed with this knowledge, I am now investigating how to circumvent barriers that restrict effective treatment from reaching glioblastoma tumors. My research is part of a collective endeavor aimed at developing and assessing new immunotherapy treatments tailored specifically for glioblastoma.
The pathway toward effective glioblastoma treatment through immunotherapy is riddled with complexities. Although no immunotherapies are currently approved for clinical use in treating this malignant form of brain cancer, there is a burgeoning interest in expanding research efforts and investment. It’s crucial to recognize that immunotherapy does not uniformly benefit all cancer types; there are potential immune-related side effects, such as organ inflammation or swelling in the brain, underscoring the importance of meticulous treatment administration.
Determining an appropriate delivery method is critical. Non-invasive options, like injections into the bloodstream or spinal cord, represent substantial advancements over traditional surgical interventions. As such techniques are refined, the likelihood of improving patient outcomes increases significantly.
While glioblastoma remains a daunting foe in cancer treatment, the advances in immunotherapy spark hope for achieving more effective and targeted therapies. As research progresses, there exists a palpable sense of optimism that breakthroughs in understanding and combating this challenging disease may soon materialize, ultimately transforming the lives of those affected.