The immunoproteasome plays a critical role in the immune system’s response to external threats such as pathogens. By degrading intracellular proteins and presenting the resulting peptides to immune cells, this enzyme complex enables the immune system to recognize and respond effectively to invading viruses and bacteria. However, in certain cases, such as autoimmune diseases, the immunoproteasome can become overactive, mistakenly attacking the body’s own tissues. This paradox highlights the importance of carefully regulating the activity of the immunoproteasome to prevent immune disorders.
Researchers have long sought to identify selective inhibitors of the immunoproteasome. A significant concern in this pursuit is the potential for such inhibitors to inadvertently disrupt the broader proteasome activity within the cell, which is essential for functions like protein recycling and cellular waste management. Therefore, the development of selective inhibitors has been deemed vital not just for efficacy, but to mitigate unwanted side effects.
Advancements in Drug Development by Synthetic Biology
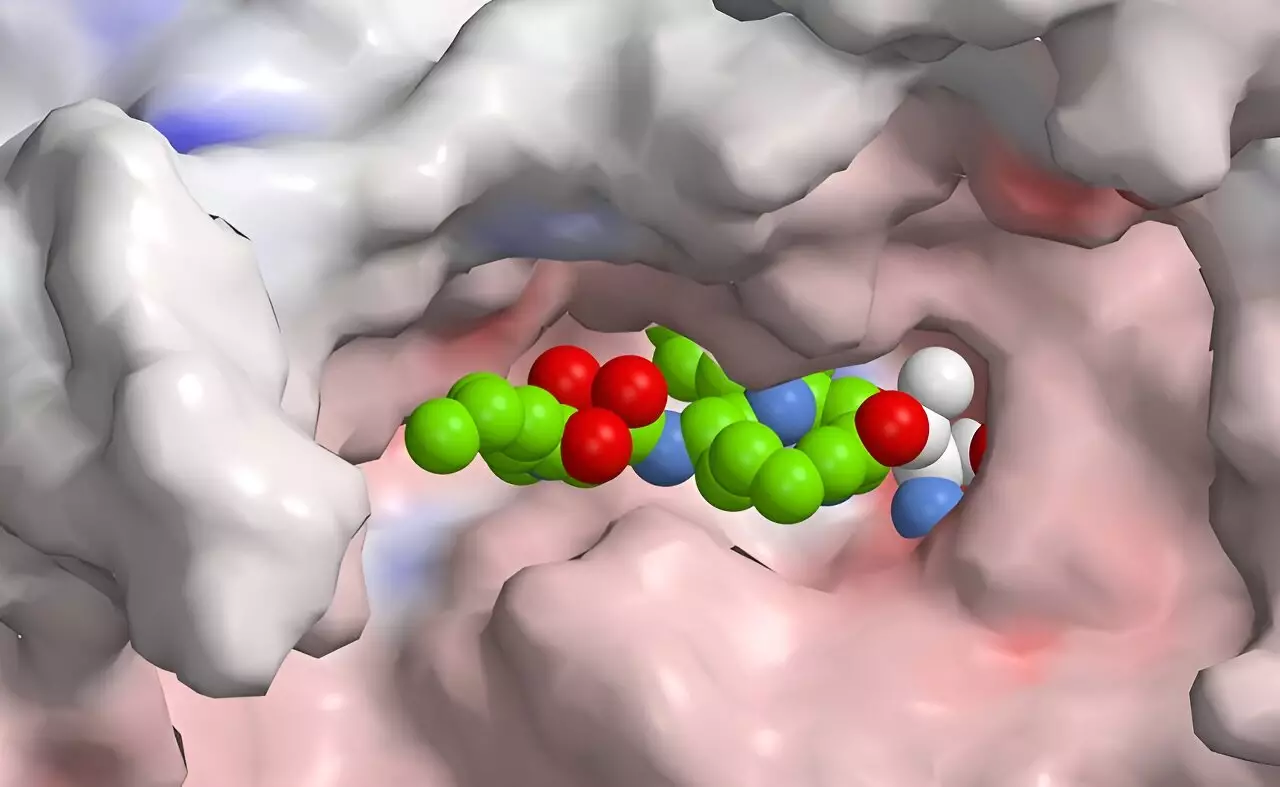
Recent advancements by a research team led by Helge Bode at the Max Planck Institute for Terrestrial Microbiology have shown promise in achieving the selective inhibition of the immunoproteasome. Through a process of synthetic biology, the researchers have engineered a method to synthesize a novel class of drugs derived from natural bacterial substances. Their innovative approach focuses on the creation of a unique drug candidate—a peptide-polyketide hybrid—that has the potential to act selectively on the immunoproteasome.
Peptides and polyketides offer valuable characteristics as therapeutic agents, with the former produced via non-ribosomal peptide synthetases and the latter through polyketide synthases. The hybrid nature of this new class of drugs allows for the fusion of functional attributes from both types of compounds, enhancing their potential utility in treating immune-related diseases or even cancer.
Bode’s team, in collaboration with scientists from Technical University Munich and the University of Duisburg-Essen, successfully assembled a peptide-polyketide hybrid in a streamlined process using XUT technology. This innovative method leverages docking sites within thiolation domains—essential components in both non-ribosomal peptide synthetases and polyketide synthases—allowing for the integration of both peptide and polyketide functionalities.
This hybrid approach is particularly noteworthy because it mirrors naturally occurring compounds, such as syrbactins, which are produced by certain bacteria to impair cellular functions in higher organisms. By clogging the proteasomes in susceptible cells, these substances induce cell death, a mechanism that could be harnessed for cancer therapies. Despite the existing proteasome inhibitors on the market, the selective targeting of the immunoproteasome remains uncharted territory, making the findings from Bode’s research a promising development in the field.
While the initial compounds created from this research are not yet sufficiently selective for practical therapeutic use, they represent a foundational step towards the development of more refined inhibitors specifically targeting the immunoproteasome. The potential to modify these compounds through computational modeling and high-throughput synthesis processes allows researchers to rapidly iterate on designs, optimizing for enhanced selectivity and reduced side effects.
This methodological advancement signifies a new era in drug discovery, where computational simulations can expedite the identification of the most promising candidates for drug development. As scientists refine these inhibitors, the anticipation grows regarding their applications in treating various autoimmune conditions and potentially reprogramming how we approach immune system modulation therapeutically.
Overall, the collaborative research led by Bode marks a transformative advancement in our understanding and manipulation of the immunoproteasome, setting the stage for more effective treatment strategies that minimize the risk of side effects while maximizing therapeutic efficacy. As research progresses, the ability to develop specific compounds for nuanced applications in immune-related diseases could change the landscape of modern medicine.