Sudden cardiac arrest represents a critical medical emergency with dire consequences. When the heart ceases to pump effectively, blood circulation stops almost instantaneously, leading to a swift onset of ischemia—particularly in vital organs such as the brain. This profoundly affects brain function, as neurons begin to suffer irreversible damage within minutes due to the lack of oxygen and nutrients. Thus, the window for successful resuscitation has traditionally been limited, compelling the medical community to seek innovative methods to extend this critical timeframe and improve survival rates following such events.
Recent investigations by a team led by Dr. Xiaoshun He at Sun Yat-Sen University in China have opened unconventional avenues in this field of study, offering new hope for increasing the viability of resuscitation post-cardiac arrest. Their pioneering work focuses not only on the immediate effects of brain ischemia but also on the potential restorative functions of other organs, specifically the liver. By reviving brain activity in pigs up to nearly an hour after circulation had ceased, researchers are challenging previously held assumptions about the limitations of brain recovery.
The shocking revelation from this research lies in the discovery that the liver—an organ primarily recognized for its metabolic functions—may play a crucial role in mitigating brain injury during resuscitation efforts. Past studies had acknowledged the importance of organ interactions during multi-organ ischemia, but the specific contributions of individual organs had not been thoroughly explored until now.
In carefully structured experiments involving 17 lab-raised Tibetan minipigs, researchers explored the effects of integrating a healthy liver into a life-support system designed for reviving brains subjected to ischemia. The pigs underwent a series of interventions wherein one group experienced both brain and liver ischemia while another group faced only brain ischemia, allowing the researchers to assess the protective effects of the unharmed liver. Not surprisingly, the control group, which faced no ischemia, exhibited minimal brain damage upon examination; however, a noteworthy finding was that the pigs not subjected to liver ischemia showed significantly less damage than those whose livers were also compromised.
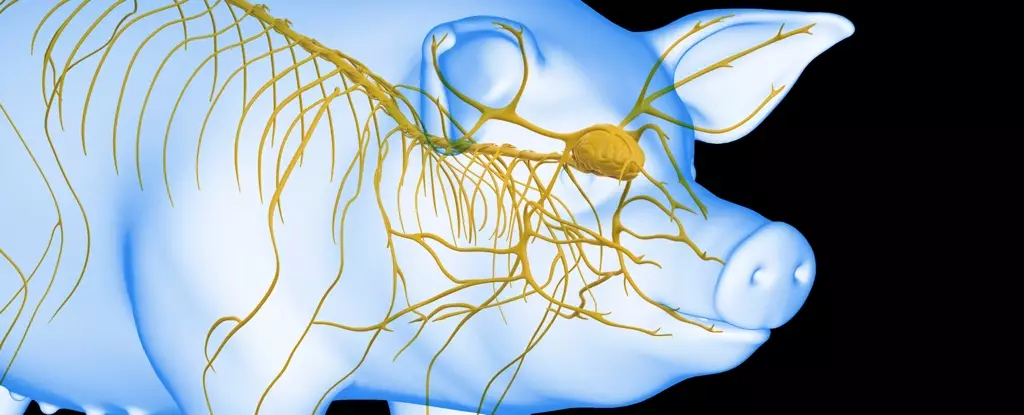
The investigation’s next phase involved a more experimental scenario: reconnecting a healthy liver to the brain of euthanized pigs through a life support system combining artificial cardiovascular support with biological recovery assistance. This method, termed liver-assisted brain normothermic machine perfusion, revealed promising results.
Researchers varied the timing of connecting the brain tissues to the life support system, starting the reconnections at intervals of 10, 30, 50, and 60 minutes following cardiac arrest. Notably, connecting the brain to the liver-supported system 50 minutes post-ischemia resulted in remarkable recoveries, including six hours of sustained electrical brain activity. Conversely, when connection occurred at the 60-minute mark, the return of brain activity lasted for only three hours—revealing the existence of a critical recovery window.
These outcomes strongly suggest that integrating a functioning liver into the resuscitation process could enhance cerebral recovery following instances of prolonged ischemia. The research indicates that the liver contributes significantly to the brain’s resilience against injury during the post-cardiac arrest period.
This groundbreaking study not only expands our understanding of organ interdependence during medical emergencies but also sets the stage for innovative research pathways that could revolutionize resuscitation protocols in humans. If the results observed in these pig models can be adapted for clinical application, the potential for extending the time frame for successful resuscitation could dramatically alter treatment outcomes for patients experiencing cardiac arrest.
The implications extend beyond mere survival; they underscore the importance of exploring organ interactions and functionalities in critical situations. As the medical community delves deeper into these findings, there may emerge more exhaustive treatment approaches that prioritize multi-organ health as part of resuscitation strategies.
The findings from China’s recent research not only shine a light on the complex relationships shared among the body’s organs during instances of ischemia but also inspire a hopeful outlook for the future of resuscitation therapies. By treating the human body as an integrated system rather than a collection of isolated parts, we may carve a path toward improving survival rates and enhancing the quality of life for those affected by sudden cardiac events. As this field of research evolves, it invites further exploration into the essential roles that various organs play in supporting critical recovery, ultimately marking a promising dawn for cardiac care.