For many individuals striving to reach and maintain a healthy weight, the cyclical pattern of losing weight only to regain it—commonly known as yo-yo dieting—remains an insurmountable obstacle. Traditional wisdom often attributes this to metabolic slowdown or psychological challenges, but recent scientific discoveries suggest an even more intricate culprit lurking within us: the microbiome, particularly the diverse bacteria inhabiting our guts. What if the key to breaking free from the vicious cycle lies not solely in willpower or calorie counting but deep within the microscopic ecosystems that influence our cravings and eating behaviors?
This emerging research challenges deeply ingrained perceptions about diet failures, pointing towards a biological mechanism that may make healthy eating habits not just difficult but biologically maladaptive after certain dietary patterns. The implications extend beyond nutrition advice, hinting at a paradigm shift in how we approach weight management—one that encompasses microbiological health alongside traditional diets.
The Microbiome: Our Hidden Enemy or Unexpected Ally?
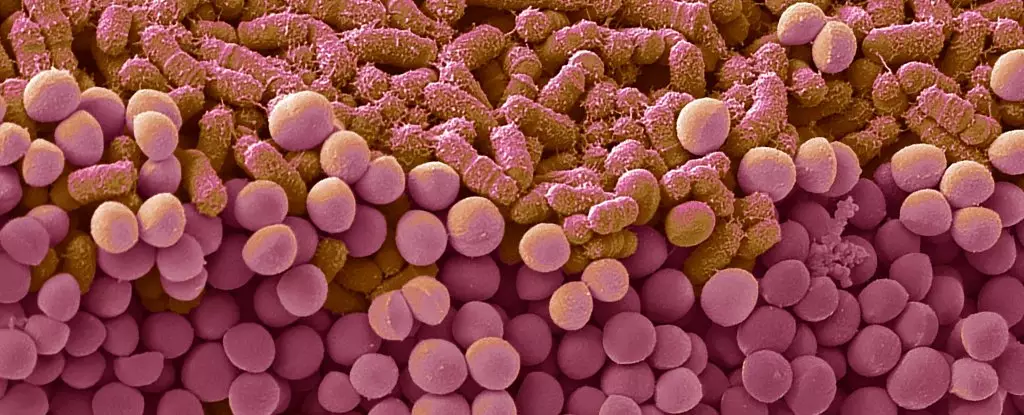
The gut microbiome—the collection of trillions of bacteria living within our digestive system—is often portrayed as a silent partner in health. However, a groundbreaking study conducted by teams from French universities provides evidence that these microscopic organisms actively shape our behaviors, especially in the context of dieting. When mice were subjected to cyclic diets alternating between normal and high-fat, high-sugar regimens, they exhibited binge-like eating behaviors once they returned to healthier food sources. Even more striking was the discovery that these behavioral shifts persisted long after the diet cycles ended.
The researchers pinpointed that these diet cycles don’t merely induce fleeting changes; they catalyze durable alterations in the composition of gut bacteria. These microbial shifts, in turn, seem to modify the animals’ metabolism and neural response to food, making pleasure-driven eating, rather than hunger-driven eating, more prominent. When the altered bacteria were transplanted into other mice, those animals also developed binge-eating behaviors, suggesting a causal relationship rather than mere correlation.
This evidence raises provocative questions: Are repeated dieting attempts inadvertently rewiring our gut bacteria in ways that undermine future efforts? Are we conditioning our microbiomes to promote disordered eating patterns that sabotage long-term weight stability?
Decoding the Brain-Gut Connection in Binge Eating
Beyond microbiological changes, the study unveiled a fascinating insight into how the brain’s reward pathways are affected by these gut bacteria shifts. The mice displayed altered brain activity associated with hedonic (pleasure-driven) eating, indicating that dieting-induced microbiome modifications might be rewiring neural circuits responsible for food reward. Essentially, after cycles of restriction and refeeding, the animals’ brains began to associate certain foods with pleasure more intensely, prompting episodes of binge behavior even in the absence of physical hunger.
This revelation brings to light the complex interaction between gut bacteria and brain function—often referred to as the microbiota-gut-brain axis. It suggests that dieting doesn’t merely influence physical health but may profoundly alter how our brain perceives and responds to food rewards. Such insights could explain why many individuals find themselves unable to resist cravings after dieting episodes, thus perpetuating the yo-yo cycle.
Furthermore, understanding this mechanism could unlock new therapeutic avenues. If the microbiota influences brain circuits governing reward and appetite, then modulating these bacteria might restore a healthier balance, reducing compulsive eating behaviors. This aligns with emerging trends in personalized medicine, where microbiome-targeted treatments could enhance weight loss success.
The Path Forward: Rethinking Dietary Interventions
While these findings stem from animal models, they undoubtedly spark critical questions for human health. If similar processes occur in humans, it could mean that traditional dieting strategies inadvertently induce microbiome alterations that make sustained weight loss difficult. It’s a humbling realization that our bodies might be fighting back on a microbial level—an insidious form of biological resistance to dieting.
To effectively combat this, future research must prioritize understanding how specific gut bacteria change with dieting patterns in humans and how these changes influence behavior. Interventions could potentially include probiotics, dietary modifications aimed at fostering beneficial bacteria, or even microbiome transplants tailored to stabilize a healthy gut ecosystem.
Moreover, it is crucial to recognize the psychological and neurobiological components intertwined with these microbiome shifts. Combining microbiome-targeted therapies with behavioral interventions might be the most promising strategy to break free from the cycle of weight regain and binge eating.
In essence, the fight against yo-yo dieting demands a comprehensive approach—one that considers the microbe-driven mechanisms underpinning our eating habits. As science continues to unravel this hidden layer of influence, the prospect of more effective, long-lasting solutions to obesity and disordered eating becomes increasingly tangible.