Recent investigations into the health of dairy workers in Michigan and Colorado have uncovered alarming yet relatively under-addressed findings related to the highly pathogenic avian influenza, specifically the H5N1 strain. In a study conducted by the US Centers for Disease Control and Prevention (CDC), blood analyses of 115 dairy employees revealed that approximately 7% harbored antibodies indicative of prior exposure to this virulent virus. Such data suggests that despite the low immediate threat to public health, the potential for mismanagement of avian influenza outbreaks could be significant.
The implications of these findings are multifaceted, indicating not only the presence of the virus but also the resilience of individuals against severe manifestations of the disease. Notably, half of those tested exhibited no symptoms at all, implying that mild infections could be more common than previously understood. This latent infection pattern raises questions about our capacity to monitor and respond adequately to emerging infectious diseases, especially in occupational settings where exposure risk is heightened.
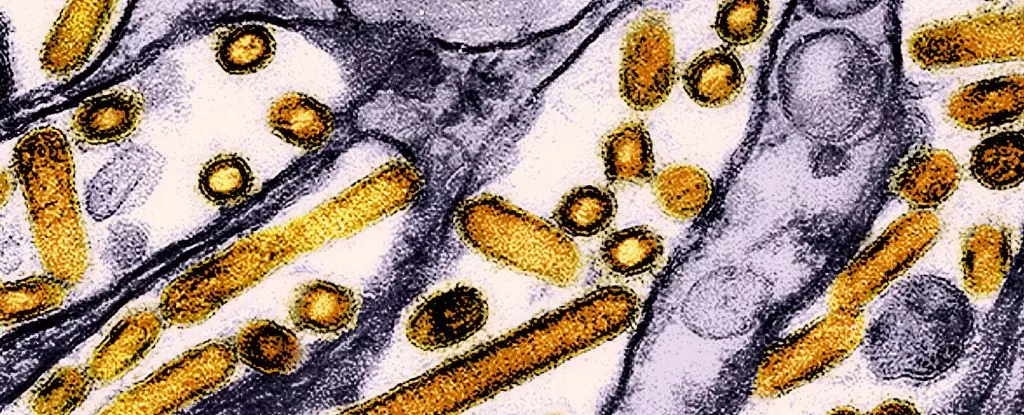
While the current infections suggest that the immediate human health risk remains low, prevailing conditions could pave the way for significant mutations. The case from Cambodia, which has drawn considerable attention, is a stark reminder of the potentially devastating evolutionary trajectory of H5N1. This particular hybrid strain has proven fatal for at least three patients and showcases mutations that elevate its transmissibility, particularly among mammals. Fortunately, human-to-human transmissions have not been reported in this Cambodian outbreak, yet the situation underscores the need for global vigilance.
Meanwhile, neighboring Canada has recorded its first human infection linked to a variant of H5N1 associated with outbreaks in US dairy cows. The affected teenager is battling a critical condition due to a strain that exemplifies genetic modifications facilitating human infection. These developments emphasize that the risk landscape of avian influenza can shift dramatically and unpredictably—reinforcing the necessity for rigorous tracking and management of infectious diseases.
An essential component of the CDC’s findings lies in the demographic of affected dairy workers. All individuals with detectable antibodies had direct roles in dairy operations; many had been involved in milking procedures or cleaning activities related to cattle. Alarmingly, reports revealed that none of these workers utilized the personal protective equipment (PPE) that health guidelines recommend for individuals handling HPAI A(H5)-infected animals.
The alarming lack of PPE usage raises ethical questions about the responsibilities of employers and the training provided to workers. Furthermore, effective outreach initiatives must be culturally relevant to address the diverse workforce dynamics, particularly among Spanish-speaking workers. The responsibility extends beyond mere compliance; it involves creating an environment where health and safety protocols are respected and substantiated.
Mitigating Risk: A Call for Robust Surveillance and Education
The findings compel public health officials to prioritize enhanced educational programs for dairy farmers and workers. Comprehensive training on the risks associated with avian influenza and proper protective measures is paramount. As the CDC emphasizes, a targeted approach to health outreach, particularly for non-English speaking communities, can play a crucial role in mitigating risks associated with infections.
Alongside initiatives for worker education, there is a pressing need for improved surveillance systems to detect avian influenza in both poultry and humans. With over 400 dairy herds infected across 48 states, proactive measures can stymie further spread and inform rapid containment strategies for both avian and potential human cases.
The urgency of these findings extends beyond human health to wildlife conservation efforts and broader ecological impacts. Since the onset of the highly pathogenic bird flu outbreak in 2022, more than 90 million domestic birds in the US alone have been culled to curtail the spread of disease. The introduction of vaccination programs for endangered species, such as the California condor, represents a critical step in addressing the ecological ramifications of avian influenza.
Simultaneously, researchers are racing to develop effective vaccines for human use. Multifaceted approaches combining veterinary public health, human health, and environmental safeguarding are essential to navigate the complexities posed by infectious diseases.
The insights drawn from recent studies illuminate a much deeper narrative around H5N1 and its unrecognized implications for human and animal health. With the potential for rapid change posing constant threats, vigilance and proactive engagement in educational and preventive initiatives are paramount for safeguarding public health against evolving pathogens.