Emerging research in cancer immunotherapy is highlighting the importance of harnessing a balanced or dual immune response to enhance treatment efficacy and patient survival rates. Two recent studies have revealed striking connections between the activation of both type 1 and type 2 immune responses and long-term remission in cancer patients. These revelations challenge conventional understandings of immunotherapy and pave the way for innovative treatment strategies that might shift the tide in the ongoing battle against cancer.
Rethinking Cancer Immunotherapy
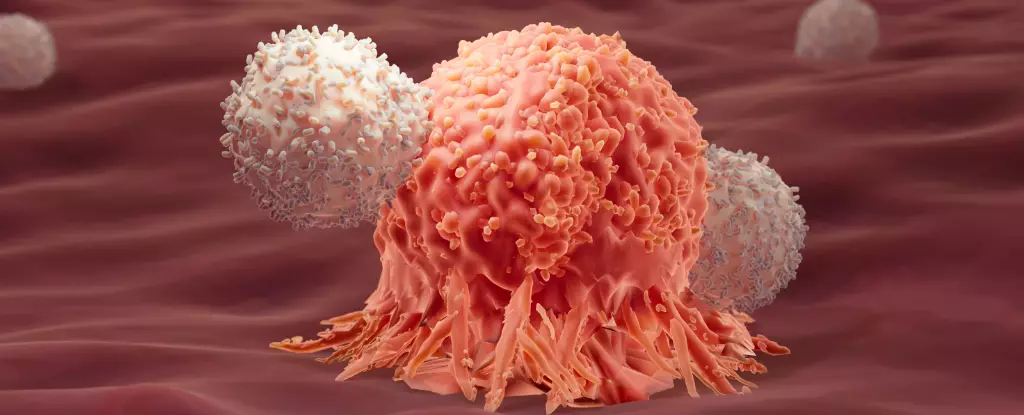
Historically, immunotherapy has been celebrated as a groundbreaking advancement in cancer treatment, leveraging the body’s own immune system to target and eradicate malignant cells. The most well-known form is CAR-T cell therapy, which involves extracting a patient’s T cells, genetically modifying them to enhance their anti-cancer abilities, and reinfusing them into the patient. Despite the promise of this technique, success rates have been inconsistent, with relapses occurring in nearly half of acute lymphocytic leukemia (ALL) patients within a year following treatment.
The recent studies investigating long-term remission cases in patients who benefited from CAR-T therapy have introduced new perspectives on why some individuals respond positively while others do not. Researchers sought to map out the characteristics of immune cells in long-term survivors, which led them to detect a compelling correlation between prolonged remission and the presence of type 2 immune response markers—an immunity typically associated with combating larger parasites rather than cancer cells.
Type 2 Immune Response: A Paradigm Shift
These findings are revolutionary, particularly because the type 2 immune response was previously deemed a liability in the context of cancer treatment. This response, attributed to the body’s way of addressing larger threats, was generally considered irrelevant or even detrimental in the fight against tumor growth. However, the new data suggests that the interplay between type 1 and type 2 responses might possess synergistic properties that enhance the body’s ability to fight cancer.
In the follow-up study involving mice with colon adenocarcinoma, researchers employed a dual approach that utilized both immune response types. Remarkably, 86 percent of the mice that received this tandem treatment were cured, indicating that an integrated immune strategy might hold the key to effective interventions even for solid tumors, which are classically resistant to immunotherapy.
Hailed as a breakthrough, this dual approach holds multiple implications for how we understand immune dynamics in the fight against cancer. Instead of solely focusing on activating type 1 responses, which specifically target cancer cells, researchers can now explore how type 2 responses can additionally contribute to sustained cancer fighting capabilities.
One of the more fascinating elements of these studies is the role of metabolic pathways in immune cell function. The researchers found that the modified type 2 immune proteins were stimulating glycolysis—a metabolic process that converts glucose to energy—thereby providing T cells with an energy boost crucial for their endurance in fighting cancer. This insight adjusts our focus from merely augmenting the immune response to ensuring that immune cells possess the necessary energy reserves to perform effectively over the long haul.
This aspect of research underscores the complexity of the immune system and its potential adaptability. It reveals that the success of immunotherapy may hinge not only upon the type of immune response triggered but also on the metabolic state and vitality of the immune cells involved.
As studies continue to unfold, the implications for these findings are profound. The concept of yin and yang in immunity suggests that integrating different immune responses can enhance overall resilience against cancer. This not only justifies further investigation into therapies that incorporate both immune response types but also encourages a shift in how clinicians approach treatment planning for individual patients.
The goal of achieving long-term remission and preventing cancer relapse could become less elusive if researchers and clinicians can design treatments that exploit these newly discovered correlations. As the field of immunotherapy evolves, it is crucial to keep pace with such insights, which offer hope for more personalized and effective approaches to managing cancer.
By revisiting the dynamics of immune responses and harnessing their synergistic potential, the landscape of cancer treatment may well change for the better. The future of cancer immunotherapy lies not solely in fortifying the body’s defenses, but also in understanding the intricate dance between different types of immunity and the metabolic pathways that sustain them.