Recent projections paint a dire picture of the future regarding antimicrobial resistance (AMR), suggesting that drug-resistant superbugs may account for nearly 40 million deaths over the next 25 years. This alarming statistic underscores a growing public health crisis that requires urgent attention and intervention. Superbugs, which are pathogens that have adapted to resist commonly used antibiotics, pose a unique challenge to healthcare systems around the globe. The groundbreaking research published in The Lancet represents the first systematic attempt to quantify the long-term impact of these dangerous organisms, shedding light on the potential mortality rates and the broader implications for global health.
Understanding the Impact of Superbugs
Infections caused by superbugs already claimed the lives of more than a million people between 1990 and 2021. These figures reveal a stark contrast when examining different age demographics; while fatalities among children under five have declined significantly due to enhanced infection control measures, the mortality rates for older adults have surged. Specifically, the death rate from superbug infections in individuals over 70 has risen by more than 80% over the past three decades. This demographic shift poses questions regarding the resilience of our healthcare ecosystems as populations age, leading to increased vulnerability to infections that are exceedingly difficult to treat.
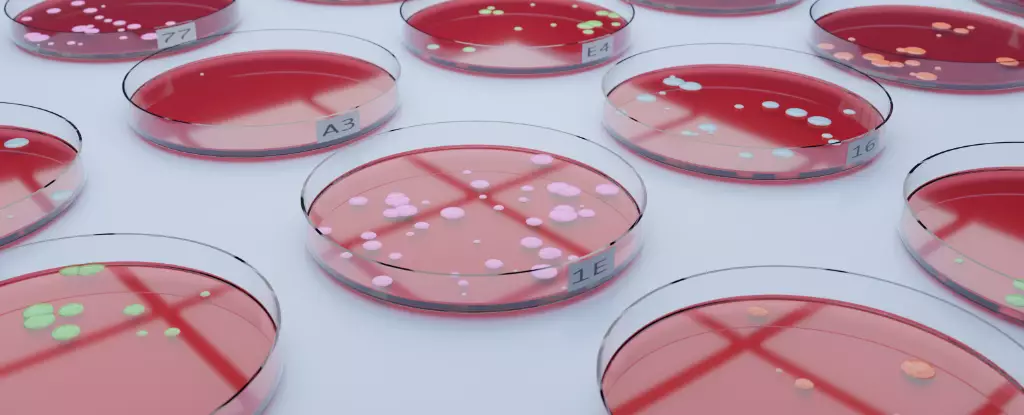
The emergence of drug-resistant bacteria, such as MRSA (Methicillin-resistant Staphylococcus aureus), illustrates the extraordinary challenge posed by AMR. The doubling of MRSA-related deaths from 65,000 to an estimated 130,000 between 1990 and 2021 indicates a sobering trend that aligns with an increase in antibiotic resistance. Such trends warrant serious reflection from policymakers, healthcare providers, and the public, as AMR continues to evolve and increase the burden on health authorities worldwide.
The researchers utilized sophisticated modelling to predict that, if current trends persist, AMR-related deaths could rise by an astonishing 67%, reaching nearly 2 million per year by 2050. Additionally, this phenomenon could contribute to a staggering total of 169 million deaths, positioning AMR not only as a cause of death but as a significant factor in global mortality rates overall. However, this grim outlook is not an inevitability; the model also suggests alternative pathways. If substantial efforts are made to improve antibiotic stewardship and access to effective treatments for severe infections, it is estimated that 92 million lives could be saved by 2050.
This dichotomy emphasizes that while AMR presents a formidable challenge, there is still an opportunity for intervention and improved health outcomes worldwide. Collaborative efforts among governments, an emphasis on proper antibacterial use, and investment in medical research can positively influence the trajectory of AMR and mitigate its potential impact.
The phenomenon of antimicrobial resistance is partly natural but significantly exacerbated by human activities. The indiscriminate use of antibiotics across various sectors—from healthcare to agriculture—aggravates the situation, fostering an environment where superbugs can thrive and proliferate. Misuse among the general public, such as failing to complete prescribed courses of antibiotics, further contributes to the cycle of resistance.
Awareness and education are crucial in changing behavior related to antibiotic use. Public health campaigns must inform individuals about the dangers of overusing antibiotics and the role they play in developing resistance. By fostering a greater understanding of AMR, societies can shift towards more responsible antibiotic consumption.
As world leaders prepare for a high-level meeting on AMR at the United Nations, this research serves as a crucial reminder of the impending dangers posed by drug-resistant pathogens. It is imperative that we collectively prioritize action against AMR through innovative strategies, robust healthcare policies, and awareness campaigns.
The threat posed by superbugs is real and requires immediate global attention. By understanding the ramifications of AMR and fostering collaboration among healthcare professionals, governments, and the public, we can work toward a future where antibiotic resistance does not decimate populations but instead remains a manageable public health issue. The time to act is now—our collective health depends on it.