The COVID-19 pandemic revealed the severity of infectious diseases in a way that nothing else could. While many had heard about viruses and bacteria before, the global crisis transformed abstract concepts into urgent realities. Central to understanding pandemics is the concept of transmissibility—how easily a pathogen can jump from one person to another. Such insights are not just academic; they have profound implications for public health, personal safety, and societal resilience.
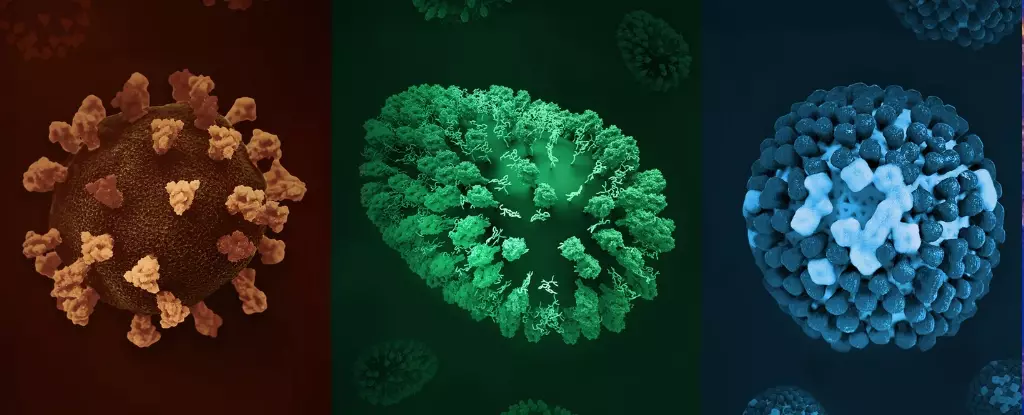
At the core of disease transmission lies a nuanced interplay between biological factors and social behaviors. Variability in how pathogens spread is vast, from airborne viruses that linger in the air to those that require close and prolonged contact. Recognizing these differences underscores the importance of scientific comprehension in crafting effective responses. For instance, a pathogen’s R0—or basic reproduction number—serves as an essential indicator of its contagiousness, revealing the average number of people one infected individual can infect in a fully susceptible population.
What becomes immediately apparent upon examining R0 values is that some diseases are astonishingly tenacious. Measles, for example, boasts an R0 ranging between 12 and 18, indicating its extraordinary ability to spread. Remarkably, this high infectivity means that a single case can rapidly escalate into hundreds or thousands of infections if unchecked. Conversely, diseases like tuberculosis, with R0 values sometimes below 1, spread more slowly and require prolonged contact, exposing different vulnerabilities based on environmental and social factors.
Beyond Numbers: The Implications of Disease Transmission Dynamics
The significance of the R0 metric extends beyond mere statistics; it influences strategies for containment and prevention. High R0 diseases place a premium on vaccination programs, strict quarantine protocols, and behavioral changes. Measles exemplifies this necessity. Despite the existence of an effective vaccine, declining vaccination coverage due to misinformation, complacency, and disruptions like COVID-19 have led to alarming resurgences. The disease’s airborne nature, combined with its low infectious dose, makes it a prime example of why herd immunity—achieving a high proportion of immunized individuals—is crucial. When vaccination levels drop, the door opens for outbreaks that can spiral out of control rapidly.
On the other end of the spectrum, diseases such as tuberculosis demonstrate that less contagious infections can still pose significant threats, especially given their complicated treatment regimens and growing drug resistance. TB spreads primarily through prolonged close contact, and the presence of drug-resistant strains complicates treatment efforts, often requiring lengthy, complex, and costly therapies. The slow nature of TB transmission and its ability to hide within the body for years exemplify how lower transmissibility does not equate to lower danger.
Moreover, understanding transmission routes clarifies the limited but severe risks posed by diseases like Ebola. While Ebola’s R0 estimates (around 1.5 to 2.5) are modest compared to measles, its case fatality rate can reach 50% or higher. Its primary mode of transmission through bodily fluids underscores the importance of physical contact precautions. Though less contagious than airborne diseases, Ebola’s severity demands targeted containment strategies rooted in transmission understanding.
Protecting Society by Grasping Transmission Secrets
An essential lesson revealed through scientific study and recent outbreaks is that controlling infectious diseases hinges on insights into how they spread. Vaccination remains the cornerstone of prevention, but personal behaviors and environmental hygiene are equally critical. For highly contagious airborne diseases, measures such as mask-wearing, ventilation, and diligent hand hygiene are non-negotiable. Conversely, for infections transmitted through prolonged contact or bodily fluids, limiting close interactions and practicing safe hygiene are crucial.
Understanding the dynamics of infectiousness also fosters empathy and responsibility. Recognizing that some pathogens can be transmitted before symptoms manifest, as with measles or COVID-19, emphasizes that even asymptomatic individuals may unwittingly propagate disease. This knowledge pushes society toward universal precautions and repeated public health messaging, which are vital for controlling outbreaks.
Finally, the intricate understanding of disease spread informs policies that balance individual liberties with community safety. It underscores the importance of herd immunity, not只是 for protecting vulnerable populations but also for ensuring societal stability. When vaccination rates dip, these dormant threats can resurface with vigor, reminding us that public health is a collective endeavor grounded in scientific literacy.
By delving into the mechanics of infection transmission, we gain a powerful tool—not just for responding to ongoing health crises but also for preventing future ones. It’s an investment in knowledge that pays dividends in lives saved and communities protected. Recognizing that every handshake, every touched surface, and every cough carries potentially deadly consequences should motivate us to be more vigilant, more informed, and more committed to safeguarding our collective health.