The unfortunate reality surrounding cardiac arrests is that survival often hinges on immediate action. When a person goes into cardiac arrest, time is of the essence, and bystander intervention through CPR (cardiopulmonary resuscitation) can be lifesaving. However, studies indicate a troubling disparity in the willingness to perform CPR based on the gender of the victim. An analysis of CPR response rates has shown that bystanders are less likely to provide assistance to women compared to men, exposing a potential gap in emergency response that warrants urgent attention.
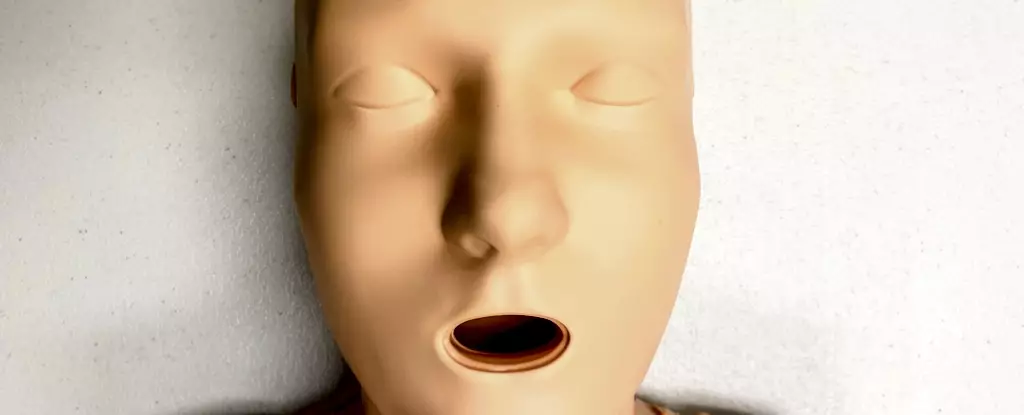
A comprehensive Australian study that scrutinized 4,491 cardiac arrest cases revealed that only 65% of women received CPR from bystanders, in stark contrast to 74% of men. Essentially, this translates into a reduced chance of survival for women in these critical moments. The underlying reasons for this discrepancy are multi-faceted, ranging from social perceptions to the design of CPR training materials. A notable factor is the prevalence of CPR training manikins, which, strikingly, are predominantly flat-chested. With 95% of CPR training manikins failing to represent women anatomically, there is a significant risk that this lack of representation translates into practical hesitation during real-life emergencies.
While the actual technique for performing CPR remains unchanged regardless of breast presence, the psychological barrier posed by the absence of realistic training tools might influence bystanders’ decisions to act. Research suggests that the design and representation of training materials play a crucial role in the confidence and readiness of potential responders. When training is primarily male-oriented or features a default male physique, it may inadvertently suggest that only men require urgent care during a cardiac arrest, thereby perpetuating gender biases in emergency responses.
The implications of this bias extend beyond the immediate urgency of a CPR emergency; they reflect a broader trend in healthcare inequalities affecting women, transgender, and non-binary individuals. Women experiencing cardiac issues often face greater dismissals or misdiagnoses, resulting in delayed treatment and poorer health outcomes. Furthermore, women are statistically less likely to survive CPR, and if they do, they are at a higher risk for sustaining brain damage—a dire consequence of receiving delayed resuscitation efforts.
The societal implications are staggering. While cardiovascular diseases are the leading cause of death among females worldwide, the healthcare system continues to struggle with disparities that put women at a distinct disadvantage. Understanding these patterns calls for immediate structural changes in how CPR training is approached, and it emphasizes the essential need for an inclusive approach to healthcare.
Several psychological barriers contribute to the gender bias seen in CPR response rates. Bystanders may feel uncomfortable about the prospect of touching a woman’s body during resuscitation efforts, fearing misunderstandings about their intentions or concerns over potential legal repercussions. Misinterpretations of physical contact can lead to inaction during critical moments when every second counts.
In simulations designed to assess intervention responses, researchers found a tendency for bystanders not to prepare a woman for resuscitation by removing clothing, demonstrating a clear bias. These findings illustrate how deeply ingrained cultural norms can deter potentially lifesaving actions.
While the fear of being accused of inappropriate behavior is valid, it highlights the crucial need for community education that emphasizes the importance of CPR and the need to prioritize lives over social fears.
As the data suggests, incorporating gender-sensitive approaches into CPR training is paramount. This can include the development of diverse manikins, such as those that are anatomically representative of women, larger body types, and individuals of various ethnic backgrounds. Only through the creation of a comprehensive range of training tools can we effectively challenge existing biases and encourage inclusivity in CPR training.
Research initiatives should focus on understanding how various demographic factors impact bystander behavior. Enhanced education about how to recognize cardiac arrest—regardless of the victim’s gender—could significantly increase intervention rates. Furthermore, empowering individuals with the knowledge that they do not need to perform unnecessary actions, such as removing clothing unless absolutely vital, can alleviate fear and hesitation.
The disparate response to female cardiac arrest victims during CPR emergencies is rooted in a combination of cultural, educational, and representational issues. The need for comprehensive, inclusive CPR training materials cannot be overstated. We must ensure that all individuals, regardless of gender or body type, receive equitable emergency assistance when most needed. Addressing these issues will not only improve survival rates but may usher in a new era of understanding and empathy in cardiac response practices, ultimately fostering a society where every life is valued equally.