Herpes Simplex Virus Type 1 (HSV-1) is primarily recognized for causing cold sores, yet recent research illuminates a more insidious aspect of this ubiquitous virus—its potential to invade and damage the brain. Groundbreaking studies led by teams from the University of Colorado and the University of Bourgogne in France have aimed to dissect the mechanisms through which HSV-1 infiltrates the central nervous system (CNS). This exploration not only seeks to chart the virus’s path but also to understand its implications for neurodegenerative diseases, a connection that has begun to attract serious academic interest.
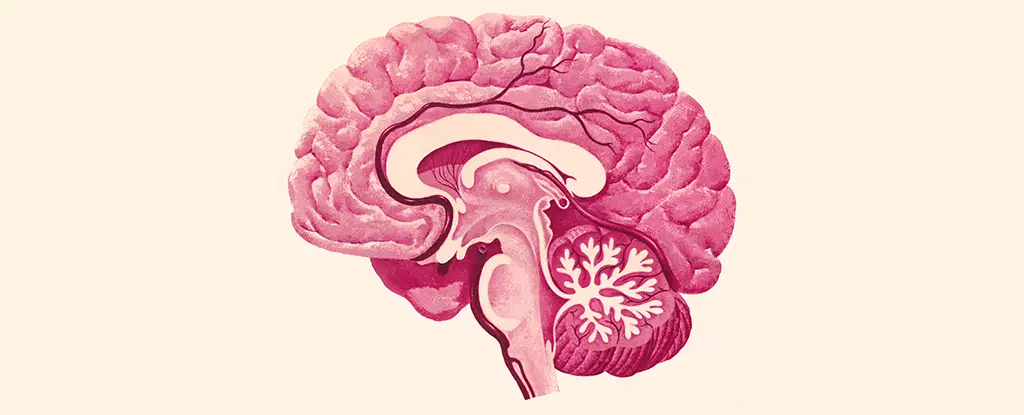
Traditionally, HSV-1 is known to enter the CNS either via the trigeminal nerve or the olfactory nerve. However, the precise ways in which it propagates once inside the brain remain elusive. The research conducted evaluated how HSV-1 affects various brain regions, an essential endeavor for grasping its role in degenerative conditions. As neurology expert Christy Niemeyer from the University of Colorado pointedly notes, “Identifying how HSV-1 can get into the brain and what brain regions are vulnerable is key in understanding how it initiates disease.” This suggests that a detailed mapping of viral spread in CNS could unveil critical insights into both the mechanisms of infection and its potential consequences.
The findings from the recent study revealed that HSV-1 predominantly affected crucial areas such as the brain stem and the hypothalamus. Each of these regions plays vital roles in vital functions including autonomic control of heart rate, respiratory patterns, mood regulation, and hormonal balance. Intriguingly, other significant regions like the hippocampus—critical for memory—remained unaffected by the viral infection. This selective impact raises intriguing questions about the virus’s relationship with various cognitive deficits and diseases, especially in the context of Alzheimer’s disease, which is characterized by memory impairment and has seen recent associations with HSV-1.
The study also delved into the behavior of microglia—the immune cells primarily responsible for maintaining homeostasis in the CNS. Microglial activation was observed in response to HSV-1, presenting characteristics of inflammation. Notably, prolonged microglial activation outlasted the viral presence, hinting at chronic inflammation’s detrimental potential. Chronic inflammation is increasingly recognized as a common denominator in various neurological conditions, including Alzheimer’s. Thus, the interplay between HSV-1 infection and subsequent microglial responses may be a critical factor in understanding neurodegenerative disease pathology.
The interconnection between HSV-1 and neurodegenerative diseases, particularly Alzheimer’s, prompts important considerations regarding chronic inflammation and its consequences. Niemeyer’s observations suggest a correlation between persistent cellular inflammation from HSV-1 and the acceleration of cognitive disorders. “Persistently inflamed cells can lead to chronic inflammation, a known trigger for a number of neurological and neurodegenerative diseases,” she emphasizes. This indicates that the viral infection may not directly incite conditions like Alzheimer’s, but rather exacerbate existing vulnerabilities.
The pivotal findings from this study mark a crucial step towards unraveling the complex relationship between HSV-1 and various neurological conditions. While more research is necessary to clarify these associations, these insights provide scientists with foundational knowledge to design future studies aimed at therapeutic strategies that might block the virus’s entry into the brain or mitigate chronic inflammation. As we cultivate a deeper understanding of HSV-1’s role within the CNS, the prospects of improved interventions to combat the potential neurodegenerative consequences it harbors become all the more feasible.
In sum, HSV-1 is not merely a virus limited to causing cold sores; it stands as a critical player in the research landscape concerning brain health. As science continues to investigate this connection, a clearer picture of how common viral infections may significantly impact neurological disorders is expected to emerge.