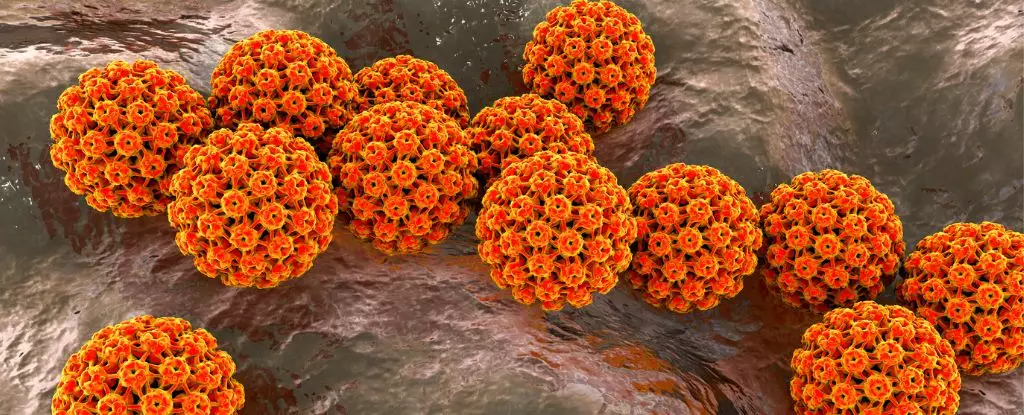
Recent research underscores a pressing public health issue: men are increasingly susceptible to oral human papillomavirus (HPV), a virus closely linked to the development of oropharyngeal cancers. While HPV has long been recognized for its role in cervical cancer among women, the focus on male susceptibility, particularly in later life, is gaining significant attention. By identifying men as a high-risk group, public health efforts can pivot toward improving vaccination coverage, especially among those who missed earlier opportunities, potentially mitigating the alarming rise of HPV-related cancers in various regions globally.
The Alarming Trend of Oropharyngeal Cancer
Oropharyngeal cancers, primarily affecting the throat and mouth, have reached epidemic proportions in places like the United States and Europe, with men being diagnosed at rates far exceeding those of women. This alarming trend persists even in individuals devoid of traditional cancer risk factors such as smoking or excessive alcohol consumption. Research has indicated that a significant portion of these cancers can be traced back to preventable infections, specifically strains of HPV, namely HPV-16 and HPV-18, which are implicated in up to 90% of oral cancer cases.
Additionally, the latest combined evidence from studies across the US, Brazil, and Mexico emphasizes a critical caution: men remain vulnerable to new infections throughout their lives, not just in youth. This revelation accentuates the need for proactive health measures, particularly vaccination, to combat this silent epidemic.
Age and Susceptibility: A Paradigm Shift
Historically, public health messaging has suggested that HPV vaccination is most beneficial when administered at a young age, suggesting limited efficacy and diminishing returns for older males. However, the findings of recent studies challenge this notion, demonstrating that the risk of acquiring HPV does not diminish with age. This suggests that ongoing vaccination efforts for males, particularly beyond the standard age limits, could be instrumental in preventing future infections and, consequently, cancer development.
This shift in understanding calls for broader age-based vaccination strategies that do not confine their focus solely to young males, but rather embrace a more inclusive approach that encompasses middle-aged men, who may also be at risk yet have been largely overlooked.
The Vaccination Gap: An Opportunity for Change
Despite clear evidence supporting the efficacy of the HPV vaccine in reducing cancer risks, particularly strains HPV-16 and HPV-18, vaccination rates among males remain startlingly low compared to their female counterparts. This disparity raises critical questions about public health strategies and outreach efforts aimed at increasing immunization rates.
To tackle this, it’s vital for health organizations, like the US Centers for Disease Control and Prevention (CDC), to emphasize the importance of HPV vaccination among all genders. Enhanced educational campaigns that effectively communicate the risks associated with HPV and the benefits of vaccination, especially addressing the misconception that HPV is a female-only concern, could play a key role in bridging the vaccination gap.
One of the challenges in addressing oral HPV infections is the misunderstanding of transmission methods. While sexual contact remains a significant risk factor, it isn’t the sole mode of transmission. Research suggests that HPV can also spread through non-sexual contact methods, including skin-to-skin contact and even via fingers and oral interactions. This nuance complicates public health messaging, yet it also opens avenues for improved preventative strategies.
The recent study from the Moffitt Cancer Center reinforced this complexity by revealing that nearly 20% of the male participants examined had prevalent oral HPV infections, indicating a substantial burden of disease at the baseline. Notably, the presence of HPV-16 was prevalent among individuals with specific risk factors, including alcohol consumption and sexual behaviors. This profile calls for targeted interventions that identify at-risk populations and encourage informed discussions around HPV prevention.
As the incidence of HPV-related oropharyngeal cancers continues to rise, the implications are clear. Public health responses must adapt and evolve, prioritizing comprehensive vaccination strategies that encompass all vulnerable demographics. Greater awareness, alongside targeted educational endeavors, could lead to increased vaccination uptake and ultimately diminish the incidence of HPV-associated cancers. The need for vigilance against oral HPV infections is paramount, requiring concerted efforts from both healthcare providers and communities to safeguard future generations. The fight against oral HPV is ongoing, and the stakes could not be higher.