The menstrual cycle is not just a physiological process associated with reproduction; it has profound effects on the very structure and function of the brain. A groundbreaking study led by neuroscientists at the University of California Santa Barbara has provided new insights into how hormonal fluctuations during the menstrual cycle can reshape the brain’s architecture. This research is essential as it opens avenues for understanding the important yet overlooked connection between a natural biological process and neurological health.
Neuroscientists Elizabeth Rizor and Viktoriya Babenko led a meticulous investigation tracking 30 menstruating women as they experienced various phases of their menstrual cycle. The aim was to explore not only the behavioral outcomes associated with hormonal changes but to delve deeper into how these fluctuations dynamically alter brain structures. Interestingly, this study is pioneering in its intent, marking the first reports of concurrent changes in brain-wide structures mirroring hormonal ebbs and flows. The significance of their findings lies in the potential that these brain-hormone interactions extend beyond the well-known areas regulated by the hypothalamic-pituitary-gonadal (HPG) axis.
Despite menstruation being a universal experience among individuals who menstruate, there exists a notable knowledge gap surrounding its impacts on brain development and cognitive function. Much research has centered on the cognitive aspects of hormone interactions, while attention to structural changes has been scant. Rizor, Babenko, and their colleagues pointed out that the cyclic changes in hormones, particularly those relating to the HPG axis, could lead to both observable and potentially significant changes in brain structure—an area ripe for exploration.
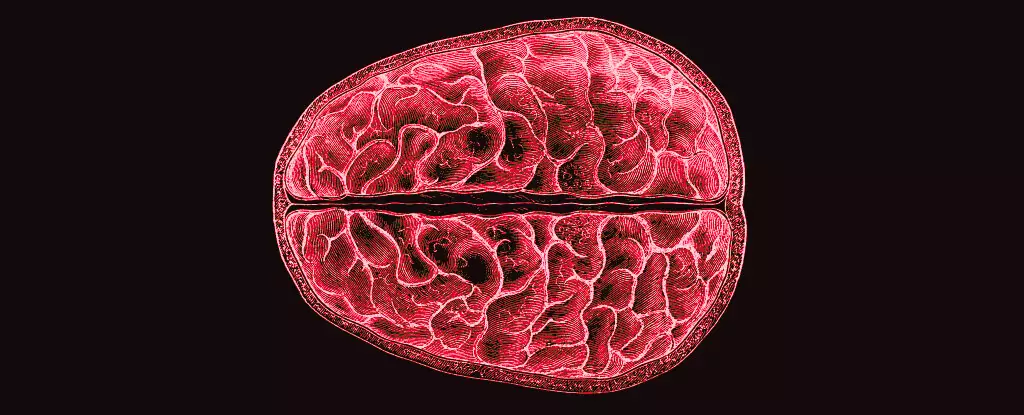
At the heart of this research is the understanding that white matter—composed of myelinated neuronal fibers—acts as a communication network between regions of gray matter. Historically, changes in this microstructure have been associated with life stages such as puberty, pregnancy, and menopause, but research examining these fluctuations specifically in relation to the menstrual cycle has been largely absent. Recognizing this gap, the researchers employed MRI technology to observe participants’ brain structures across three distinct menstrual phases: menstruation, ovulation, and mid-luteal.
The findings revealed that as hormone levels shifted, there were significant alterations in both gray and white matter volumes, as well as changes in cerebrospinal fluid levels. Notably, the period leading up to ovulation—characterized by spikes in hormones such as 17β-estradiol and luteinizing hormone—was associated with structural adjustments suggestive of enhanced information transfer capabilities within the brain. Conversely, the increase in follicle-stimulating hormone and its correlation with thicker gray matter underscored the complexity of hormonal influences.
The implications of these alterations are profound, especially when considering the psychosocial challenges faced by menstruating individuals. Research indicates that menstrual cycles can exacerbate certain mental health issues, thus understanding the brain-hormone interaction could illuminate the mechanisms behind these phenomena. For example, the observed increase in tissue volumes associated with progesterone and a decrease in cerebrospinal fluid might correlate to the fluctuating moods observed throughout the cycle.
While this research lays a solid foundation for further exploration, it raises more questions than answers. What do these changes mean for cognition, emotional well-being, and overall mental health? Are certain structural changes predictive of mood disturbances or affective disorders that some individuals experience cyclically?
Ultimately, the study by Rizor and Babenko urges a reevaluation of how we understand hormonal fluctuations—not just as peripheral biological phenomena but as key factors influencing neurological health. Bridging the knowledge gap in menstruation’s impact on the brain may lead to more comprehensive approaches in mental health support and provide opportunities for targeted interventions tailored to the unique experiences of those who menstruate. As research continues to unfold, we can hope for deeper insights that acknowledge the intricate dance between hormones and the human brain.